Peri-Implantitis

Scientific background
Peri-implant infections are pathological conditions surrounding dental implants. Mucositis refers to inflammation and ulceration in the soft tissues around an implant and is a reversible host response to periodontal pathogens. Peri-Implantitis, the destructive inflammatory process affecting both soft and hard tissue surrounding a dental implant, is more severe and leads to bone loss1.
The typical signs and symptoms of the diseases, as discussed in various consensus conferences, can be described as follows2-8:
Mucositis
- Bleeding on probing
- Redness and swelling of soft tissue
- No loss of supporting bone
Peri-implantitis
- Crater-like bone defect
- Bleeding and/or suppuration on probing
- No implant mobility
- >4 mm peri-implant probing depth
A reliable diagnosis of peri-implantitis requires the simultaneous presence of all above listed signs and symptoms. A single feature alone is not sufficient for the diagnosis.
Treatment of peri-implantitis
Peri-implantitis should be treated systematically. Bacterial plaque removal with surgical and/or non-surgical therapy is essential to prevent further progression and prepare the defect for regenerative procedures9.
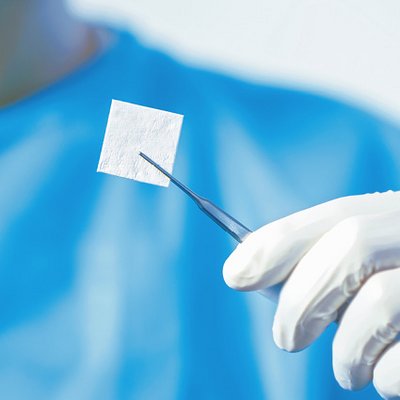
Guided bone regeneration with Geistlich Bio-Oss® and Geistlich Bio-Gide® regenerates the osseous defect after implant surface decontamination10.
References:
- Lang NP, et al.: Ann Periodontol 1997; 2(1): 343-56 (Clinical study).
- Mombelli A, et al., Clin Oral Implants Res 2012; 23 Suppl 6: 67-76 (Systematic review).
- Lang NP, et al., J Clin Periodontol 2011; 38 Suppl 11: 178-81 (Systematic review).
- Lindhe J, et al., J Clin Periodontol 2008; 35(8 Suppl): 282-85 (Clinical study).
- Mombelli A, Criteria for success. Monitoring In: Proceedings of the first European Workshop on Periodontology, (eds.) N.P. Lang & T. Karring, pp. 317–325. London: Quintessence 1994 (Book chapter).
- Mombelli A, Prevention and therapy of peri-implant infections. In: Proceedings of the 3rd European Workshop on Periodontology, (eds.) N.P. Lang, T. Karring & J. Lindhe, pp. 281–303. Berlin: Quintessenz Verlag 1999 (Book chapter).
- Tomasi DP & Derks J, J Clin Periodontol 2012; 39 Suppl 12: 207-23 (Systematic review).
- Zitzmann NU & Berglundh T, J Clin Periodontol 2008; 35(8 Suppl): 286-91 (Systematic review).
- Schwarz F & Becker J, Peri-implant Infection: Etiology, Diagnosis and Treatment. Quintessence Publishing 2007 (Book).
- Schwarz F, et al., J Clin Periodontol 2009; 36(9): 807-14 (Clinical study).
Regenerative treatment of peri-implantitis
A systematic review of regenerative measures following anti-infection treatment revealed that peri-implantitis lesions can be effectively filled with bone substitute materials1. Geistlich Bio-Oss® provides more radiographic bone fill in peri-implant lesions compared with autogenous bone2.
When defect fill of peri-implantitis defects is required, use of Geistlich Bio-Oss® in combination with a Geistlich Bio-Gide® membrane results in marked clinical improvement3.
References:
- Renvert S, et al., Clin Oral Implants Res 2012; 23 Suppl 6: 84-94 (Clincal study).
- Aghazadeh A, et al., J Clin Periodontol 2012; 39(7): 666-73 (Clinical study).
- Schwarz F, et al., J Clin Periodontol 2009; 36(9): 807-14 (Clinical study).
Regenerative treatment of peri-implantitis
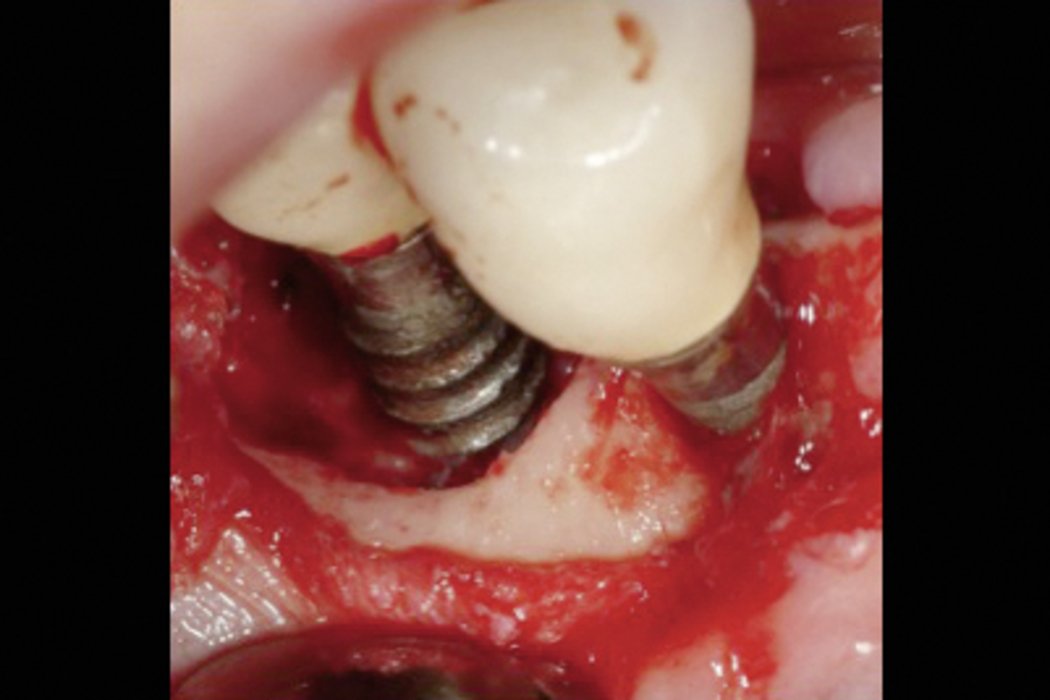
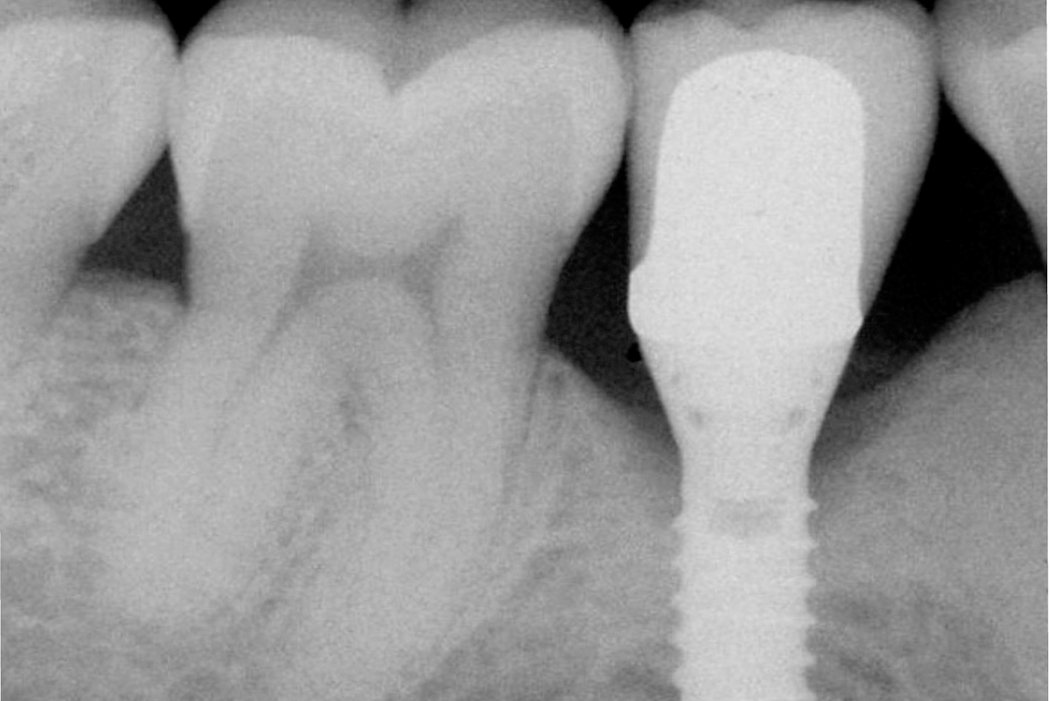
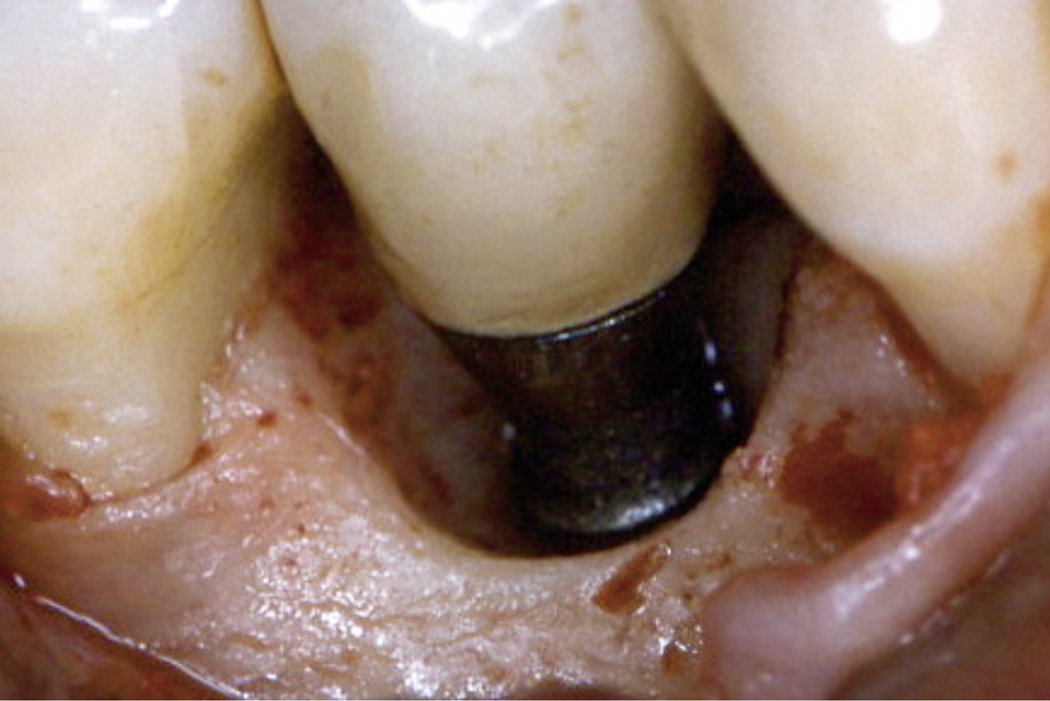
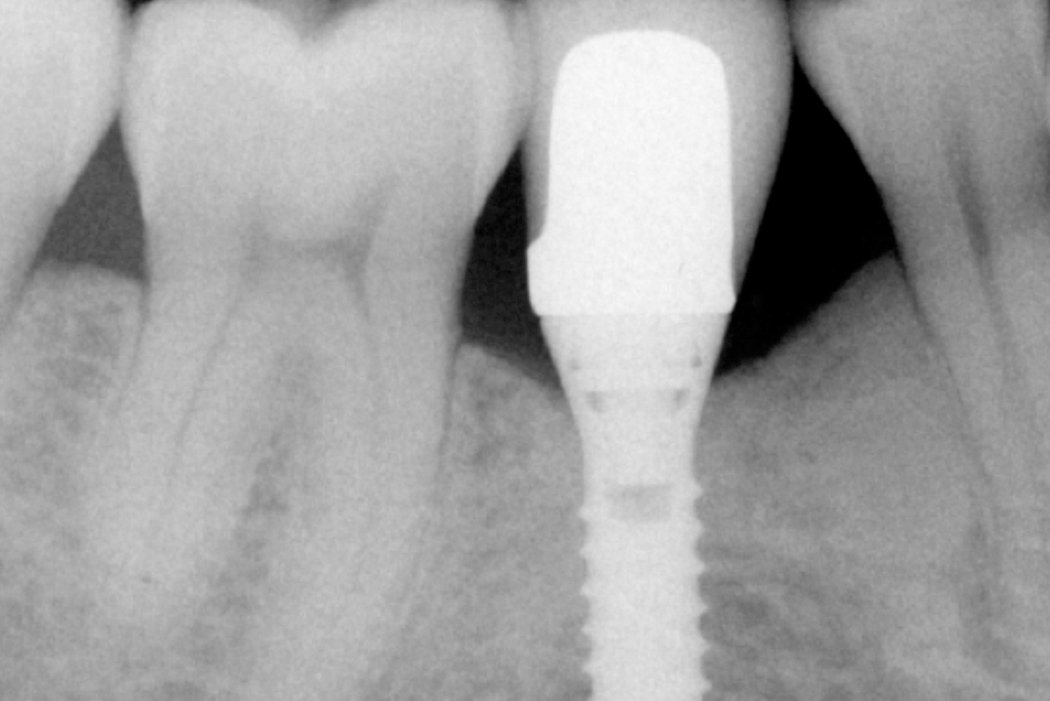
Clinical Case
Surgical regenerative treatment of a peri-implant bone defect with a favourable long-term result.
Defects caused by peri-implantitis can be corrected with Geistlich Bio-Oss® bone replacement material in combination with a Geistlich Bio-Gide® membrane.
References:
- Renvert S, et al., Clin Oral Implants Res 2012; 23 Suppl 6: 84-94 (Clincal study).
- Aghazadeh A, et al., J Clin Periodontol 2012; 39(7): 666-73 (Clinical study).
- Schwarz F, et al., J Clin Periodontol 2009; 36(9): 807-14 (Clinical study).