AMIC MTP

AMIC® Chondro-Gide® in the 1st MTP Joint
Chondral lesions of the first metatarsophalangeal joint (MTP1) are a common pathological condition of the foot. Left untreated, they can progress to hallux rigidus, causing pain and functional impairment. There are controversial opinions about the optimal treatment of chondral defects in the MTP1 joint. Some support the joint preserving (distraction, cartilage regenerative techniques, OATS, osteotomies) and others the joint sacrificing (arthrodesis, arthroplasty) techniques.
In a large, prospective, consecutive, non-controlled case series, 198 patients with chondral lesions of the MTP1 joint who were treated with AMIC® plus peripheral blood concentrate (PBC) were studied. Most patients also had a deformity that was treated concomitantly. The authors compared the 5-year results with their previously reported 2-year results. 1
References:
- Richter et al. 2022, Foot Ankle Surg 28(8) (Clinical study)
- Nurmukhametov et al. 2020, Cartilage (13(1) (Clinical study)
- Rajeev et al. 2023, Foot Ankle Surg 29(2) (Clinical study)
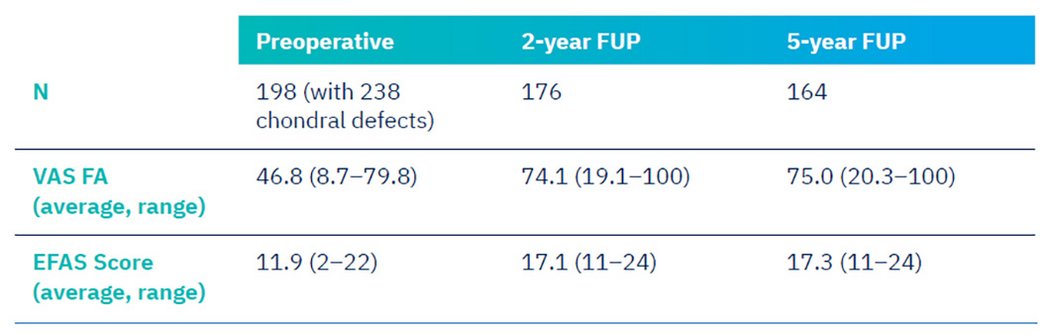
The table shows the number of patients (N) available for 2- and 5-year follow-up with their pain and EFAS scores at the two follow-up time points. The scores improved markedly compared to preoperative values, but there was no difference between the 2-year and 5-year results.
The authors concluded, that AMIC®+ Peripheral Blood Concentrate as a treatment for chondral defects at MTP1 as part of a joint-preserving surgery resulted in improved and high validated midterm outcome scores.1
Another study with a smaller cohort analyzed VAS, AOFAS and FFI in 19 patients after AMIC® in the first MTP joint due to osteoarthritis (OA). The patients have been followed-up for 3, 6 and 12 months after the surgery. The results showed that a first MTP joint AMIC® procedure can be a fairly effective method of surgical treatment that can relieve pain and significantly improve the quality of life of patients with first MTP joint OA.2
References:
- Richter et al. 2022, Foot Ankle Surg 28(8) (Clinical study)
- Nurmukhametov et al. 2020, Cartilage (13(1) (Clinical study)
- Rajeev et al. 2023, Foot Ankle Surg 29(2) (Clinical study)
AMIC® Chondro-Gide® in the Lesser MTP Joints
Freiberg’s disease affects young patients and can lead to second MTP joint arthrosis early in life. This can have detrimental long-term effects on the patient’s function and affects the quality of life. The overall prognosis for Freiberg’s disease remains uncertain. There is not a single procedure that has demonstrated consistent long-term good outcomes. Systematic review studies have concluded that both joint preserving and joint sacrificing procedures have poor or insufficient evidence for effective treatment for Freiberg’s disease. Getting the younger patients return to full activity is of utmost importance. The treatment described enables the remodelling of the affected metatarsal head and changes the local environment for the cartilage regeneration process triggered by AMIC® Chondro-Gide®.
A published case series involved ten patients who underwent this surgical procedure. The results showed significant improvements in pain relief and functional outcomes over the follow-up period. The mean baseline VAS improved from 26.4 (10.2 ± 42.6) to 30.3 (95%CI- 2.1 ± 58.5) at one year. The mean MOxFQ and VAS at the end of 36 months was 31.4 (95%CI-6.6 ± 57.2) and 47.3 (4.3 ± 80.3) respectively. Thus, the authors conclude that bone grafting combined with an AMIC® procedure appears to be a promising treatment option for patients with Freiberg's disease.3
References:
- Richter et al. 2022, Foot Ankle Surg 28(8) (Clinical study)
- Nurmukhametov et al. 2020, Cartilage (13(1) (Clinical study)
- Rajeev et al. 2023, Foot Ankle Surg 29(2) (Clinical study)